 X-rays of Don Schiel's shoulder before (left) and after (right) the procedure performed by UCH orthorpedic surgeon Jonathan Bravman, MD.
X-rays of Don Schiel's shoulder before (left) and after (right) the procedure performed by UCH orthorpedic surgeon Jonathan Bravman, MD.
Don Schiel was diagnosed with rheumatoid arthritis (RA) 20 years ago and has lived with debilitating joint pain for the last decade. He worked telecommunications jobs in Boulder and Westminster until six years ago, when the pain disabled him.
“Every joint hurts, from the jaw down,” said Schiel, 47, of Westminster. “There is never a day without pain, but you learn to live with it.”
But Schiel discovered his pain threshold late last summer. His arthritic left shoulder was in such bad shape that lifting his hand to his mouth to stifle a yawn sent him into spasms of agony. If he simply tried to stretch his left arm, the shoulder easily popped out of joint. The RA had so damaged the tendons and cartilage, he said, that he could slide the shoulder back in place without much effort. Then he went back to another cycle of pain.
Orthopedic surgeon Jonathan Bravman, MD, shows a model of the technology he used for a new shoulder replacement technique. A “transfer device” (left) that fits into the scapula provides a guide that is based on the patient’s anatomy.
 Orthopedic surgeon Jonathan Bravman, MD, shows a model of the technology he used for a new shoulder replacement technique. A “transfer device” (left) that fits into the scapula provides a drilling guide that is based on the patient’s anatomy.
Orthopedic surgeon Jonathan Bravman, MD, shows a model of the technology he used for a new shoulder replacement technique. A “transfer device” (left) that fits into the scapula provides a drilling guide that is based on the patient’s anatomy.
Today, the left shoulder is one place Schiel no longer feels the wrath of RA, thanks to a total shoulder replacement performed at University of Colorado Hospital by orthopedic surgeon Jonathan Bravman, MD. Bravman planned and completed Schiel’s surgery with new technology designed to improve the chances of nestling the components of Schiel’s new shoulder joint with maximum precision.
Real view
The technology, from Vista, Calif.-based DJO Global, uploads preoperative CT scans of the patient’s shoulder to software that produces a three-dimensional image of the entire anatomical structure. The surgeon uses the image to plan a “virtual procedure,” as Bravman put it, that offers far greater procedural certainty than ever before.
That’s a key to decreasing the risk of later surgical revisions caused by a less-than-ideal fit. It’s not easy to reach the ideal – one that accommodates back-and-forth tilt, rotation, and angle between the ball at the head of the humerus (upper arm) and the cup of the glenoid (the cavity at the edge of the shoulder bone, or scapula) – with a joint as complex as the shoulder.
“I can plan the heck out of the procedure, and measure the placement within micrometers,” Bravman said. He did so for Schiel, examining the computerized model of his ruined left shoulder. The procedure wouldn’t be terribly complicated, in Bravman’s view, but for such a young patient, the new shoulder “would have to last extra long, leaving very little room for error,” he said.
Reliable guide
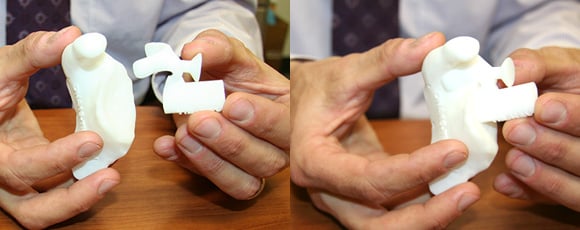 A model of the transfer device (left) hooked to a model of the scapula.
A model of the transfer device (left) hooked to a model of the scapula.
At the time of the surgery, Bravman fitted a “transfer device” to Schiel’s coracoid, a small hook-shaped structure at the end of the scapula. The device, manufactured on the basis of the CT images of the Schiel’s shoulder, provided a drilling guide for Bravman to place the implant.
Bravman called the transfer device a surgical “template” that helps increase surgeons’ confidence that “we are doing what we think we are doing.” The more precise the measurements, the better the ball-and-cup fit for the new joint, and the better the surgical outcomes, he said. Conversely, an imprecise fit means the joint may wear unevenly, much like the tires on a badly aligned car.
“The technology gives me a way to have access to 3-D information relative to the patient’s anatomy,” Bravman said. “That’s critical to the placement of the components in a way that is not otherwise available in standard care.”
Breaking new ground
Schiel is thus far the only patient to undergo shoulder replacement with the new technology at UCH, which Bravman said is the first in the state to use it. He said Schiel’s case was a trial he hopes will lay the groundwork for full approval from the hospital’s OR Products Committee.
Bravman conceded the system could slightly increase the cost of procedures at the front end, but he maintained that could be offset easily if it reduces the incidence of failures that require additional surgeries.
“We’re in the infancy of this,” Bravman said, “but I fully agree with the idea.”
As for Schiel, he requires no convincing. He got a referral from UCH rheumatologist Duane Pearson, MD, in January to see Bravman, who performed the procedure Feb. 4. Two-and-a-half months later, he said his left shoulder is pain-free. He completed a physical therapy regimen at AF Williams, but said the post-operative pain was minimal.
“Compared with what I experienced before, it was nothing,” he said. “My left shoulder is the only part of my body that doesn’t hurt.” He said he’s now considering a second procedure on the right shoulder to prevent it from deteriorating as seriously as the left.
Shouldering a heavy load. For Schiel, being able to stretch his left arm and pick up a cup or fork with his left hand is a huge relief. But the benefits of the surgery were more than physical. An enthusiastic athlete who played soccer, football, and other sports growing up in California’s Bay Area, Schiel said the worsening RA forced him to give up the physical activities he enjoyed. That, in turn, took a mental toll.
“I went from being an athlete and an outgoing person to the point that I didn’t want get out of bed or move,” Schiel said. “I try to stay positive and I don’t like to complain, but it becomes a psychological battle.”
He still has many physical challenges and relies on a variety of medications to manage his RA, but the surgery helped to lift his depression. “I know I can get up and do something,” Schiel said. “Your attitude and the way you think changes the way you’re living.”
Schiel said he was initially hesitant about the surgery, but was “blown away” by Bravman’s work and grateful for his effort to explain the procedure and to make him comfortable with giving it a try.
“I can’t express how happy I am with how it went,” Schiel said. “It’s made me hope that there is a chance that other things can be dealt with.”




